West Coast autumn…
Hope you have a good weekend everybody!
Your Custom Text Here

Photo credit: Sharon Lefkov
West Coast autumn…
Hope you have a good weekend everybody!

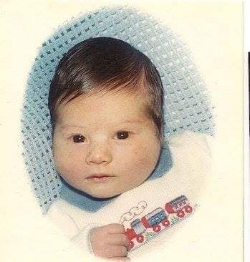
Terrell & Holly two days before he took his life.
My son, Terrell Anthony Scott, suffered from schizophrenia and other mental health issues. At the age of five, Terrell tried to hang himself.
Terrell was incarcerated at Northampton County Prison located in Easton, Pennsylvania from 2009 to 2014 without having a warrant against him, and no jurisdiction either.
The prison medical team ignored Terrell's mental health issues. They ignored Terrell's cries when he was being raped, beaten, bullied, and asking for medical treatment for being exposed to another prisoner's HIV infected blood. Terrell's pleas to go to trial were all ignored.
Terrell was accused of sexually assaulting three girls, punching their faces repeatedly, striking their teeth with a claw hammer (not one tooth was damaged), and a list of other horrible crimes.
Terrell tried to take his life while in Northampton County Prison. He ended up on life support for over dosing his medication with his saved saliva. It took Terrell over four weeks to save up enough saliva to kill himself.
Terrell then spent two-and-a-half years at State Correctional Institution at Retreat located in Hunlock Creek, Pennsylvania. During his incarceration at SCI, Terrell tried to take his life again. He swallowed two razor blades, then took another razor blade and cut his neck from ear to ear three times and cut both his wrists, up to his forearms, 12 times. Again, Terrell's mental health issues were ignored.
Terrell did not commit the crimes he was accused of committing. This is how I know:
A) During the time Terrell was around the said victims, two Easton children and youth caseworkers came to the house twice a week. They made no mention of any form of abuse.
B) At school, neither the girls' teachers, the school nurse, nor the guidance counselor made mention of any form of abuse.
C) Mandated workers at the summer nights program, which a pastor ran, made no mention of any form of abuse.
D) My former boss, who is a hairdresser, saw the girls. They made no mention of any kind of abuse.
Terrell endured several years being away from his family, his only support system. He was held down by other prisoners while one inmate beat Terrell's head repeatedly, and suffered permanent hearing loss and loss of eyesight. He was paraded around naked at Northampton County Prison and thrown in the hole for months because other inmates lied about him. The list goes on.
Terrell completed his incarceration on August 8, 2016. He was registered as a sex offender under Megan’s Law, and put on special probation requiring him to pay for lie detector tests on a monthly basis. All the while, his mental health issues weren’t being addressed.
On August 20, 2016, Terrell took over 60 pills to kill himself. When his body rejected all those pills, he put a garbage bag over his head, secured it around his neck with jumbo rubber bands, and suffocated to death. Terrell's little brother, Amari, found him early that morning (the worst day of my life) but it was too late.
Terrell first asked me way back on December 26, 2009, "Mommy, if anything should happen to me while I'm in prison, please clear my name.” He said this right before he got beaten up. Over the years while Terrell was incarcerated, he would ask me the same thing again and again. Terrell's last plea, in his goodbye video, was to help clear his name.
Thank you so much for your interest in helping me clear Terrell's name.
Holly Alston
fairlingsdelight@aol.com
Note: Click on link: Terrell Scott’s goodbye video, made two days before he took his life, is on Youtube.
Mitchel John
Thirty-four years ago, this young man was born into a difficult world with a slew of problems. He couldn't catch a break. His first few years he struggled with upper respiratory infections, pneumonia, infectious croup, and bronchitis. He spent a great amount of time in and out of hospitals.
By age four, he had a developmental team working with him and was diagnosed with neuro-motor disability and learning disabilities. The doctors agreed this stemmed from injuries at birth. Mitchel was lifeless when he was born and had to be resuscitated. They (the docs) believed part of his brain had been damaged, even though the spinal tap done on my newborn baby came back inconclusive.
Skipping ahead to grade school, Mitchel was in special needs classes and did best when he was with a teacher one on one. If that schedule became disrupted he couldn't function. At the same time, Mitchel's gross motor skills were taking many years to develop. When riding a bike, peddling, or doing anything that required these skills, he became distraught.
Skipping ahead to high school, Mitchel’s paranoia started. He was afraid to enter the school for fear of getting lost and not being able to find his way around. I finally decided to look into an alternative high school for my boy. This was the best decision for him. He still struggled but not nearly as much.
At age 18, Mitchell joined the United States Army and other symptoms began to show — delusions, psychosis, paranoia, anxiety. I lumped it all into the fact that he was getting ready to leave for boot camp. But that wasn't the actual case. Mitchel made it through boot camp and was sent to Kentucky where he turned up missing. AWOL.
Mitchel lived, homeless, in Washington State and Los Angeles — underneath bridges and behind dumpsters. Two years passed before I saw him, again, in person. I didn't recognize him. His hair had grown down his back, he smelled terrible, and he was wearing two different shoes that looked like he'd found them in a trash can.
Moving ahead, we received the diagnosis of paranoid schizophrenia after an extensive psychological evaluation. Puzzle pieces began fitting together. Things started making sense. For me, anyway.
These past ten years have been brutal on all of us. My girls didn’t have their brother to dance with at their weddings or, now, to shoot the shit with in general.
Hospitalization is much better than jail. Mitchel has been an inpatient since 2012 with a brief discharge, last summer, for about three months. We want, more than anything, for him to get better and we know it's possible his symptoms could go away, at least for a short time. We've seen it happen before. The scary part is not knowing where or when the symptoms will return. And we know they will. Eventually.
Another year of not getting to spend a birthday with my baby boy. He's 34. He was 25 when he was admitted to Utah State Hospital. Time and schizophrenia have been cruel to Mitchel John.
Happy birthday, sweet boy. I love you forever.
Note: On November 6, Sherry and her family were able to spend time with Mitchel to celebrate his birthday — one month late.

Mitchel John

Photo credit: Marisa Farnsworth
Frog heaven.
Hope you have a good weekend everybody!

Monica writes: Twenty years ago, we were moving from Finland. Mika was sad to leave his leopard geckos behind. His only consolation was that he could get two pet rats (Bert & Ernie) once we were in the States. This is my favorite photo of him. His eyes were so trusting of us.
9/30/2018
I normally don't write anything about what is really going on in our family but currently I am more aware that I need to be a better advocate for our son. The following is an excerpt from an article by Liza Long in the Huffington Post that I want to pass on:
Recovery is an unrealistic standard for any chronic illness, including mental illness. We would never apply the blanket expectation of recovery to any other chronic illness or disability. With cancer and autoimmune disorders, we use the term “remission” to describe a life-threatening systemic illness that with luck and treatment has been stopped in its tracks. With other chronic illnesses like diabetes, we talk about managing the illness. But with mental illness, we expect people to “choose” recovery, even when they are experiencing psychosis, or when their disease steals their ability to make rational choices.
Behavioral health is an important concept for everyone. We should all focus on our behavioral health: on diet, exercise, mindfulness, good sleep habits. But behavioral health is not mental illness. Mental illness is physical illness. For people with serious mental illness, behavioral health alone will not “fix” or “cure” the chronic condition, and for us to expect otherwise is unrealistic and cruel. We need to focus on effective treatments, not inaccurate judgments about what we “believe” or “feel” mental illness is. It’s a very real health challenge, with real and sometimes devastating consequences for those who live with it and their families.
Let’s keep talking about behavioral health for everyone. But let’s stop talking about recovery for serious mental illness and start celebrating people whose brain disorders cause them to live with health challenges comparable to those experienced by cancer patients. The word we need, in the face of so much loss, is hope. Mental illness is not a choice. But hope is. Even in the face of tragedy, today I choose hope.
10/5/2018
Our son, Mika, was diagnosed with schizophrenia this summer. We knew he was ill for a few years but didn't know what it was. He decided that he couldn't live with this disease and took his life Wednesday night. Time has stopped yet the world is still turning. My heart is beating but my body feels like stone. Everything feels like a contradiction. We are well acquainted with sorrow and know that grief is just love with no place to go.
Note: Monica lives in Montana.

Monica writes: About ten years ago, this photo was taken of Mika on the lake near the summer house. It kind of represents his reality and broken reality in the reflection.

Joe last winter.
10/7/2018
My son, Joe, hasn’t been doing well. He’s off his meds and is psychotic.
We've had Joe 5150d twice in the last 30 days. This last time seemed like they were trying to place him in a long-term in-patient treatment. He was in a two-week facility. Last Sunday my son called because it wasn’t going well and he was arguing with staff. He said, “They’re going to discharge me.”
Long and short of it. I was under the impression that he would be either in the hospital for 72 hours or at longer-term treatment, but yesterday evening I got a call from the police. “Your son is in the streets and needs to get home.” He was an hour's drive away. So we went to get him.
Joe was discharged because the "professionals" couldn’t figure out how to deal with him. What a system. Now he’s talking his usual nonsense, but I’m just happy I know where he is and where he’s getting his next meal. He’s home.
Please pray for us all. It's what we’re all dealing with. No real help out there.
10/8/2018
Since bringing Joe home yesterday, after he was discharged and homeless for a week, he’s been psychotic and rambling. Today, however, he’s becoming destructive. He screamed at my husband, pushed him, and said, “I have AIDS.” He took a queue ball from the pool table and threw it at the front window. He missed but it hit and shattered my work laptop.
We called the police but my son was gone when they arrived. The officer said, “Call us when your son returns.” We called the "non-emergency" number, as we were told, when we received location information about my son. The dispatch said, “We’ll assess him and move on if he’s not a threat.” I pointed out that Joe destroyed our property and is in need of treatment. I was told, "Statuses change. If he is evaluated as non-threatening, we'll move on."
I don't know what to do at this point because, if he comes home, we can’t have him destroying things and help doesn’t arrive when we call. In addition to his schizophrenia, Joe is using other drugs. I’m frustrated and heartbroken. I can’t help my son get the help he needs. We’re being refused, essentially. Why, why, why?
10/9/2018
My son returned home after yesterday's incident. Once again, he was confrontational so I called 911 with urgency about the situation. A cop showed up. He was aware we’d been calling previous days and basically made the assessment that there’s nothing he could do. “The destruction of your property happened yesterday. Today he’s not a threat.” He offered the option of getting a restraining order against our son so, if he violates it, he can be arrested.
What’s wrong with this picture? My son can get a criminal record but no mental health treatment. This is a vicious cycle that can be broken but only with mandatory mental health treatment. Joe’s been psychotic at the hospital and in front of the cops, but nothing can be done. They tell me.
10/10/2018
I received a call from a detention center. My son was arrested for petty theft and released. He’s not been seen or heard from since. All I can do is pray that, somehow, he manages on the streets.
10/21/2018
A few days ago my son called. Finally. He was at a mental health hospital. He said he was there for four days, but I know they only hold for 72 hours. No word since then. I worry all the time. In the evening, when I'm in bed, random areas of my face tingle and swell. From the stress I'm sure.
10/22/2018
As suspected, my son was discharged from the mental health hospital. When? They won't tell us. They say, “He's not a patient here.”
10/24/2018
Praise God. Yesterday was a low point for me with worry, guilt, and heartache. I cried, I prayed, and this morning my son called. He said he was tired and wanted to come home. He was in Yorba Linda which is about an hour’s drive for us. Don't know how he wanders the streets in the wrong direction. We picked him up, got him a burger, and brought him home. He was discharged on Monday (10/22) and said he was making his way to the coast (beach) but just got tired. "When I’m homeless, I can't sleep, I’m afraid of what someone will do.”
I asked, “How do you get by on the street?”
“I drink a lot of water, mostly, and ask for money only when I’m extremely hungry. I don't ask people for money unless I really need to. It's hard being homeless.”
I told Joe he doesn’t have to be homeless, but he feels like he has no choice because we "harass" him at home. Of course, that is the perception for him.
Another positive, while driving home, there was a call from a nearby (to our home) behavioral clinic, where Joe has an appointment tomorrow morning. He looked better than I expected, so that’s a relief. He seemed calmer, though he was still having audible hallucinations and bouts of laughter. These last few months have been the worst for him. I hope we get him the help he needs and he complies.
10/27/2018
No real treatment. This week we located our son, brought him home and took him to an appointment at a behavioral clinic. He refused to let us go in so we were shut out. His interaction at this appointment lasted, maybe, five minutes. He came out agitated.
Joe doesn't believe he needs treatment. He paces around the house 24/7, demands money, — we don't give any — and threatens to leave and be homeless. We tell him that’s his choice. I'm exhausted.
Today, he went to an AA/NA meeting somewhere and caused a scene, then went to a local bar and caused a scene there, too. He was threatening people. Police were called but never showed. My husband received a call from someone who knows my son's situation. He went to the bar to find out what happened and returned home. My son was home, too, by then. We asked, “How was your day?” He said, “I didn't do much.”
At the moment we’re just letting him be. Interactions are at a minimum. My son’s in his state of mind and not a thing we can do.

Joe after a week on the street.
Note: Viviana lives in California.

Photo credit: Paula Lozar
Aspens on a cloudy day…
Hope you have a good weekend everybody.
I have struggled with this post, but my husband, Steve, and I discussed it last night and decided we want to help educate, to the best of our ability, and to help make sense of some of the madness that surrounds us.
For a while, we knew that, in Illinois, a person has the right for a jury to determine their continued treatment in an inpatient psychiatric setting. We faced a six-person jury with an alternate to determine continued treatment for our child. We worried and dreaded the situation for weeks. How could six people, who had no experience or comprehension of this illness, determine our loved one's care? It seemed to me that a qualified physician should make that determination.
Well, yesterday, we arrived at the courtroom at 9:30 A.M. and left around 5:30 P.M. The decision was for continued treatment. I admit, after being sequestered ourselves, for five-and-a-half hours, we were frustrated and angry. But, after all was said and done, we realized that the world view of seven more individuals was changed forever. They were educated on the illness as well as the insufficiency of services in our state. One juror looked at us and said, “My heart breaks for you.”
I post this to say that, sometimes, we must be vulnerable and transparent for others to comprehend the nature of the beast we deal with, and for changes to be made. We’re not alone. Too many families live this pain. Please pray for change in our country for the care of some of our most vulnerable.

Jacque & Steve

Monica
This is the story of the loss of our beautiful Monica, age 26. She was a great artist and jewelry designer. She was generous, loving and caring. She passed away at the room and board that was her residence. Unfortunately, she suffered from ulcerative colitis, diagnosed at age 11. She also had depression issues and high anxiety. Monica spent way too many days, weeks, and months in and out of hospitals for physical and mental health issues.
Monica was living in an unlicensed room and board in Elk Grove, California. This room and board was supposed to be one of the better homes according to Heritage Oaks in Sacramento. Heritage Oaks had screened the person running it and the home. For the first four or five months, Pompae, the man running the home, was around. Monica was stable and well balanced from her medications. Pompae prepared meals for the six people living in the home. He supervised issues that came up among the residents.
Then Pompae decided he needed more income and took a job doing construction work. He’d make breakfast for everyone and go to work early in the morning. He instructed our daughter to make lunch for all of the people living in the home. Monica worried about the other people and became anxious if she wasn’t around to make the lunches. This was not her responsibility. Pompae didn’t pay her to do this. He gave her some extra kitchen privileges. My point is six people, who all had mental health issues, were left on their own all day long. Monica said sometimes they wouldn’t have dinner until 9 P.M.
The day before Monica passed away, I talked to her on the phone and she seemed to be doing okay. She was getting over a bad cold but was less stuffed up. She may have mixed up or taken too much of her prescription medications. We haven’t received the toxicology report yet. I think Pompae may have checked on her once during the night since her roommate was worried about her. He left for work at 6:30 A.M. When her roommate couldn’t wake Monica up at 9:30 A.M., she called Pompae and he told her to call 911. The paramedics arrived at 10 A.M. They worked on our daughter for an hour but couldn’t get her to breathe again. My husband and I received a call from the police department that afternoon. The worst call of our lives.
Pompae shouldn’t be running a room and board but, after talking to APS (Adult Protective Services), I’ve learned there is very little accountability and few regulations these room and boards need to follow. Many of them are just collecting rent.
This needs to change.

Artwork by GG Burns/Artist/Mental Illness Advocate
Of the season…
Hope you have a good weekend everybody!